Chapter 9 – Preventative foot surgery in diabetes
Chapter 9 – PREVENTIVE FOOT SURGERIES IN DIABETES
The risk of developing a foot infection is extremely high once an ulcer has formed. In fact, 45% of all non-traumatic foot and leg amputations in the United States are caused by diabetes, and 30% of patients who undergo a foot or leg amputation return to the hospital for treatment of the other foot within three years. The five-year survival rate for diabetics with a leg amputation can be as low as 30%. Therefore, it is crucial to exhaust every effort to keep the foot healthy—not only to preserve limb function but also to mitigate the psychological impact of amputation.
Historically, podiatrists were called in to treat diabetic foot problems and took pride in saving many diabetics from amputation, while other surgeons often opted for major leg amputations. Foot carelessness in diabetic patients can eventually lead to a major leg amputation when the leg develops an infected neuropathic or ischemic foot. The treatment of an infected diabetic foot has traditionally centered on surgical intervention, often culminating in amputation to rescue the limb. Today, however, the focus has shifted toward preventive foot surgery that addresses structural changes and the future needs of diabetics. The goal of preventive foot surgery is to reduce the chances of developing foot ulcers and bone infections, thereby preventing amputation crises. These surgeries aim to decrease pressure points on the foot that arise from deformities such as hammer toes, bunions, and calluses, as well as to prevent ingrown toenails and ulcer formation.
It is important to emphasize that one of the major objectives of preventive foot surgery in diabetics is to reduce or eliminate excessive pressure on the foot. In diabetic neuropathy, altered sensation or complete numbness means that patients lose the protective mechanism of pain. Without pain as a warning sign, diabetic corns and calluses remain unnoticed and continue to endure pressure until the skin eventually breaks down, forming ulcers. Once an ulcer forms, it can become infected, leading to tissue necrosis and even bone infection—a process that can take only a few days in patients who are unaware of the injury due to neuropathy. In contrast, people with normal sensation experience pain that prompts them to change their gait or relieve pressure, thereby preventing ulcer formation. Because pain is our body's natural defense mechanism, its absence means that the underlying problems persist unchecked. In cases where corns and calluses contribute to ulcer formation, removal of the bony prominences may be necessary to prevent further complications.
WHO CAN HAVE PREVENTIVE FOOT SURGERY?
Not all diabetic patients are candidates for foot surgery. In my practice, patients come from across the country—and even from other countries—for possible foot surgery, but about 50% are not suitable candidates. Many of these patients are referred to vascular surgeons for an evaluation to determine if vascular surgery might improve blood flow to the foot. Unfortunately, in some cases, the vascular disease is too advanced for surgical intervention.
To qualify for preventive foot surgery, it is essential that diabetes is well-controlled. Poor blood sugar levels can lead to poor recovery from surgery. A diabetic foot that is cold to the touch, shows no hair growth on the toes, lacks good pulses, and exhibits thin, shiny skin indicates poor circulation and is not a good candidate for surgery. Any trauma to such a foot—whether from surgery or an accident—can easily lead to infection and subsequent gangrene.
Conversely, a diabetic foot that is insensitive to pain yet remains warm, with strong pulses, good skin coloration, and hair on the toes can be considered a good candidate for foot surgery. Patients with these characteristics, despite having neuropathy, benefit from surgery designed to reduce pressure on areas affected by deformities such as bunions, hammer toes, calluses, and ingrown nails.
Another very important factor for the success of foot surgery is the patient's nutritional status during the recovery period. The role of a registered nutritionist becomes crucial in ensuring that proper nutrition is maintained, which in turn supports effective healing after surgery.
NAIL SURGERY
The patient in Fig. 9-1 has a thick, deformed nail which is not only cosmetically undesirable but can be a threat from a gangrenous toe.

A toenail that has become deformed no longer functions normally and instead becomes a source of intense pressure on the toe bone. If left untreated, this pressure can eventually lead to ulcer formation beneath the thickened nail, often without the patient feeling any pain due to neuropathy. By the time pus is noticed coming from below the nail, the infection may have already advanced into the bone. In such cases, it is crucial to reduce the nail as soon as possible to alleviate the pressure; if that proves ineffective, the nail and its root should be surgically removed.
An ingrown and infected nail is a serious concern as well. Chronic infection of an ingrown nail can extend to the bone under the nail, and the resulting inflammation and infection may promote the formation of small clots in the toe, ultimately leading to gangrene (see Fig. 9-2). For patients with ingrown nails, periodic trimming is recommended before the infection penetrates the buried portion of the nail. If necessary, the nail and its root can be surgically removed for permanent eradication of the problem.
HAMMER TOE
The patient in (Fig. 9-3) has a hammer-shaped second toe. The top of the toe has intense pressure from the shoe that can easily cause ulcerations. Surgically, treated (Fig. 9-4), and there will be no more threats of ulceration.
The patient in (Fig. 9-5) presents with multiple hammer toes and a bunion—a foot deformity commonly seen in diabetic patients due to motor neuropathy and consequent weakness of the foot muscles. In patients with hammer toe, the top of the toe has intense pressure from the shoe that can easily cause ulcerations. If surgically treated, there will be no more threats of ulceration. Contracted hammer toes are subjected to excessive pressure, which leads to inflammation, callus formation, and often ulceration above the toes. Unfortunately, patients that also have poor foot circulation are not considered good candidates for foot surgery. Instead, they may first undergo reconstructive vascular surgery to improve blood flow. A few days later, they could undergo reconstructive foot surgery and ultimately healed without complications (see Fig. 9-6).
THE BUNION
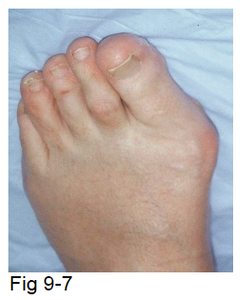
The patient in (Fig. 9-7) has a bunion deformity. The pressure exerted by the shoe on the bunion can lead to an ulcer forming over the bunion. If we remove the bunion surgically and straighten the big toe, the patient will be free of any threat (Fig. 9-8).
The pressure exerted by the shoe on the bunion can lead to an ulcer forming over the bunion. If we remove the bunion surgically and straighten the big toe, the patient will be free of any threat.
Not all diabetic patients are candidates for foot surgery. Experienced podiatric surgeons can carefully select those at high risk for developing foot ulcers for preventive surgery. If diabetes is well controlled and the foot has good blood perfusion, then preventive foot surgery may be beneficial—especially if neuropathy puts the foot at risk for ulcer formation.