Chapter 13 – Real stories. Can this happen to you? Learn from mistakes.
Chapter 13 – REAL STORIES. CAN THIS HAPPEN TO YOU? LEARN FROM MISTAKES.
Patient A – If you are diabetic, you should watch what shoe you wear
Patient A is a 47-year-old female with insulin-dependent diabetes who presented to the emergency room with an infected blister on her left foot. She reported that she had worn a specific pair of shoes (see Fig. 13-1) for a friend’s dancing party, and upon returning home, she noticed a blister on the side of her left foot. Over the next few days, the redness and pain increased, prompting her to seek emergency care.
On examination, a skin abscess was noted on her left foot with redness extending toward the ankle. The blister was incised and drained to remove the pus (see Fig. 13-2), and she was admitted to the hospital for infection treatment. Although the infection was eventually resolved, months of wound care failed to close the wound defect, leaving a large non-healing ulcer.
Due to suspicion of underlying bone infection, an MRI was ordered, which confirmed that the bone adjacent to the ulceration was infected (see Fig. 13-3). As a result, the infected bone was surgically removed (see Fig. 13-4). Within a month after the bone removal, the wound finally resolved (see Fig. 13-5), and Patient A was able to return to her normal activities.
Patient B
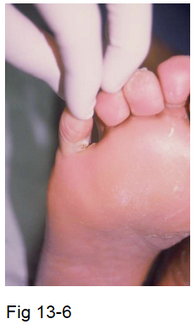
Patient B is a 55-year-old male with a 10-year history of diabetes who is on oral medications for diabetes, high blood pressure, and high cholesterol. He presented to the emergency room because the bottom of his right foot was swollen and red, even though he experienced no pain. His wife noticed a yellow-greenish, foul-smelling fluid coming from between his toes (see Fig. 13-6).
On examination, there was significant swelling and pus accumulation at the bottom of his foot. In the emergency room, the affected area was incised with a scalpel to drain the pus (see Fig. 13-7). The source of the infection was identified as the area between the little toe and the adjacent toe, which had been compromised by a fungal infection known as athlete’s foot, along with callus formation. The bacterial infection from this area had spread into the sole of the foot, causing the accumulation of pus.
Patient B was admitted to the hospital for treatment of his foot infection. Due to severe circulation problems, he was evaluated by a vascular surgeon, who determined that the infection would be difficult to heal without improving blood flow. Consequently, he underwent a revascularization procedure to enhance circulation to his right foot. Following revascularization, the wound gradually healed, although complete healing took several months (see Fig. 13-8). Without the improvement in circulation, the wound would not have healed, and he likely would have required a leg amputation.
Patient C – Lost a leg because I had ingrown toenail???
Patient C is a 67-year-old male with non-insulin-dependent diabetes, a history of kidney failure on dialysis, and severe circulation problems. He also has a long history of cigarette smoking. He initially presented with a chronic ingrown toenail, which he attempted to manage on his own by trimming the ingrown portion and cleaning it with alcohol and peroxide. Eventually, he sought medical attention in my office, but by that time, his toe had already become cyanotic and bluish (see Fig. 13-9).
Despite a multidisciplinary approach involving a podiatrist, vascular surgeon, infectious disease specialist, and endocrinologist, his toe progressed to gangrene, resulting in the loss of his big toe (see Fig. 13-10). Due to his advanced circulation problems, even a minor toe amputation struggled to heal. When the toe amputation failed (Fig. 13-10), half of his foot had to be amputated (see Fig. 13-11) in order to stop the spread of infection up the leg (see Fig. 13-12). Ultimately, our attempts to save his leg were unsuccessful, and he eventually underwent a below-the-knee amputation.
There are lessons to be learned here.
1. Even seemingly a minor problem such as an ingrown toenail, diabetic people can lose the leg
2. Do not attempt to treat the problem yourself.
3. Smoking cigarette causes damages to the circulation.
Patient D
Patient D is a 45-year-old construction worker with a 15-year history of insulin-dependent diabetes. One day after returning home from work, he removed his shoe and noticed that his sock was soaked with blood. He realized that he had stepped on a rusty nail which had penetrated his left foot, though he did not feel any pain at the time. Over the next few days, his wife observed that the redness was spreading up his leg from the bottom of his foot, and his second toe was beginning to turn black (see Fig. 13-13).
When he presented to the emergency room, immediate surgical treatment was scheduled. His second toe had progressed to gangrene and required amputation, and pus that was tracking up toward his leg had to be drained. His left foot was treated with a Wound Vac (see Fig. 13-14), a device used to suction out pus from deep tissues and promote healing. Although the wound eventually healed, the process took several months, as documented in Fig. 13-15.
Patient E – Lost a leg from hammer toe?
Patient E is a 65-year-old male with a 26-year history of type II diabetes who also had hammertoe problems affecting his 2nd and 3rd toes on the left foot. He was a long-term heavy smoker and suffered from several comorbidities, including COPD, kidney insufficiency, and heart problems. One day, he noticed pus emanating from a thick corn on his 3rd toe. By the time he presented to my office, his 3rd toe had already turned dark (see Fig. 16 and Fig. 13-17), indicating severe circulation problems. He was promptly evaluated by a vascular surgeon for revascularization procedures; however, despite these efforts, we were unable to save his foot. Ultimately, the patient lost his leg.